 Standard care for Obstructive Sleep Apnea (OSA) is providing a CPAP box, hose, mask and some basic education. This is expected to jump start the gold standard treatment of CPAP therapy for a lifetime. The problem with this “one-size fits all” approach is that it mirrors interventions for an acute illness (e.g., prescribing a cast followed by physical therapy education for a broken bone), which is characterized by abrupt or rapid onset, limited duration, and a single cause (usually). But OSA is a chronic illness characterized by gradual onset of lengthy or indefinite duration, multivariate causation (which can change over time), and a focus on functional status rather than individual diagnoses; moreover, cure is unlikely and long-term management of symptoms and disease consequences necessitated a “long-view” of treatment.
Standard care for Obstructive Sleep Apnea (OSA) is providing a CPAP box, hose, mask and some basic education. This is expected to jump start the gold standard treatment of CPAP therapy for a lifetime. The problem with this “one-size fits all” approach is that it mirrors interventions for an acute illness (e.g., prescribing a cast followed by physical therapy education for a broken bone), which is characterized by abrupt or rapid onset, limited duration, and a single cause (usually). But OSA is a chronic illness characterized by gradual onset of lengthy or indefinite duration, multivariate causation (which can change over time), and a focus on functional status rather than individual diagnoses; moreover, cure is unlikely and long-term management of symptoms and disease consequences necessitated a “long-view” of treatment.
This mismatched approach is one explanation for research findings that 10 to 20% of patients diagnosed with OSA reject therapy due to a poor experience the first night, and, of those who do use CPAP, 50 percent will not be using it at 30 months. Given that 80% of the population with OSA has never received an initial diagnosis, this means that under 10% of those suffering from Sleep Apnea in America are effectively treated!
Poor short and long-term adherence to CPAP is the proverbial “canary in the coal mine,” signaling that something is wrong with our approach to standard care.
To prevent the early attrition of patients, the fifth of patients who don’t continue with CPAP after their interface fitting, a personalized, comfortable mask and positive first experience with CPAP is key. In our previous blog, Material Success: How SleepWeaver Transformed the CPAP Mask Model, we detailed the attributes of a CPAP mask which promote comfort and prevent adverse side effects from the interface, and demonstrated that a skin-friendly, soft cloth option like the SleepWeaver line addresses many of the initial barriers to compliance that cause patients to give up on treatment, thus setting them up for success.
But over time, to address the attrition from patients who initially get off to a good start with CPAP research (Haniffa, 2004) has shown that psychological and educational interventions improve PAP usage more than mechanical (e.g., improved CPAP machines; humidification) and technological (e.g., compliance monitoring; mask fitting apps) interventions alone, for compliance. Since sleep apnea is a chronic condition, the real secret to making treatment work is sticking with it over the long haul. This is known as a longitudinal approach to sleep apnea management.
The latent need for a chronic care intervention serves as the context for the introduction of the Self-Management Educational Approach. Self-management education can be defined broadly as a systematic behavioral approach to help patients with chronic conditions participate actively in self-monitoring (of symptoms or physiologic processes), decision making (managing the disease or its impact based on self-monitoring), and problem solving (Shekelle, 2005). CPAP initiation and management involves a behavioral change, so why not take a behavioral approach to improving the process?
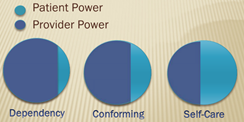 The foundation for any self-management approach is not a passive one—the emphasis is on active participation and a collaborative relationship with your provider in making treatment decisions. Self-management is successful when a patient is able to transition from dependency to collaboration with a provider. This collaboration starts with asking proactive care questions, which are detailed in this article from the American Sleep Apnea Association:
The foundation for any self-management approach is not a passive one—the emphasis is on active participation and a collaborative relationship with your provider in making treatment decisions. Self-management is successful when a patient is able to transition from dependency to collaboration with a provider. This collaboration starts with asking proactive care questions, which are detailed in this article from the American Sleep Apnea Association:
1. What is my specific diagnosis and how is it different than other sleep-related breathing disorders (SRBDs)?
2. Why do I have Sleep Apnea?
3. Request a copy of your sleep study summary report.
4. Please explain the relevance and details on my summary report.
5. Please provide me with a physical copy of my prescription for CPAP and equipment
6. What is our plan for follow up care?
7. How often do you recommend future titrations?
 Sleep Apnea Self-Management (SASM) shows you how to make the most of your collaboration with your sleep specialist and the services she can prescribe and link you to. Once you are able to establish a balanced relationship with your provider, it will be easier to work within this framework to manage the chronic nature of your condition. Research has shown that OSA affects multiple aspects of an individual’s health related quality of life, including (a) managing OSA symptoms, CPAP side effects, and weight loss; (b) maintaining work performance, social contacts, and family relationships; and (c) dealing with symptoms of depression and anxiety (Flemons, 2000; Flemons & Reimer, 1998; Veale, Poussin, Benes, Pepin, & Levy, 2002; Weaver et al., 1997). To address the heterogeneity of OSA, chronic disease self-management programs primarily focus on three content areas: (a) disease, medication, and health management; (b) role management; and (c) emotional management (Corbin & Strauss, 1988).
Sleep Apnea Self-Management (SASM) shows you how to make the most of your collaboration with your sleep specialist and the services she can prescribe and link you to. Once you are able to establish a balanced relationship with your provider, it will be easier to work within this framework to manage the chronic nature of your condition. Research has shown that OSA affects multiple aspects of an individual’s health related quality of life, including (a) managing OSA symptoms, CPAP side effects, and weight loss; (b) maintaining work performance, social contacts, and family relationships; and (c) dealing with symptoms of depression and anxiety (Flemons, 2000; Flemons & Reimer, 1998; Veale, Poussin, Benes, Pepin, & Levy, 2002; Weaver et al., 1997). To address the heterogeneity of OSA, chronic disease self-management programs primarily focus on three content areas: (a) disease, medication, and health management; (b) role management; and (c) emotional management (Corbin & Strauss, 1988).
There are formal programs available, but the following principles are a clue to how individuals can use the resources available through your healthcare provider to take control of their own health behaviors:
- What is the theory underlying the Self-Management approach?
Traditional Care: Disease-specific knowledge creates behavior change which improves outcomes.
Compared to…
Self-Management Education: Greater patient confidence in his or her capacity to make life-improving changes (self-efficacy) yields better clinical outcomes. - What is taught?
Traditional Care: Information and technical skills about the disease.
Compared to…
Self-Management Education: Skills on how to act on problems. - What is the goal?
Traditional Care: Compliance with the behavior changes taught to the patient to improve clinical outcomes.
Compared to…
Self-Management Education: Increased self-efficacy to improve clinical outcomes.
Let’s take a moment to explain how you can actualize each of these concepts: 1) With the typical approach to sleep apnea, there is a hope that learning about sleep apnea alone will change behavior. But if someone lacks confidence to stick with CPAP, all of the education in the world will not tilt the needle toward compliance. The Health Belief Model (Rosenstock, 1966) posits that people will take a health-related action when they:
- Believe that negative health outcomes are avoidable
- Believe that taking an action will avoid the negative outcomes
- Believe that they are able to take the action
- Believe they have self-efficacy (confidence in one’s ability to perform the action)
An example of this intervention is posed by patients with the following problem “CPAP is too loud; I’m not going to get to sleep.” This statement shows a lack of confidence in ability to overcome the noise barrier. Education about a state called Sleep State Misperception and learning strategies to allow noise accommodation to take place can go a long way to build hope that a patient is sleeping better than they realize with CPAP and that they can adapt to the noise from the machine and mask.
2 & 3) The self-management approach provides actual life-skills needed to act on problems with CPAP instead of simply learning the technical skills for using CPAP. This helps patients develop proficiency or “self-efficacy” to improve outcomes. The use of CPAP is a pretty straightforward process but the maintenance of its use is the tricky part. What if you develop skin irritation over time? What if the climate of the seasons has an effect on the way you tolerate treatment. How about physical changes over time (e.g., age and weight fluctuation can call for different treatment pressures or retitration)? This is where support groups come into play. You are not alone in managing issues that come up. Somewhere, someone has worked through the same barriers to compliance that you will be faced with, and having strategies to deal with them is a benefit to the group approach, aside from the obvious supportive nature of a group where you have so much in common. For example, some patients have found a “multiple mask” treatment approach works best for them for one or more of the following scenarios:
- You may prefer a nasal mask but add a secondary full face mask if you are susceptible to any condition that forces you to become a mouth breather.
- Facial pain may be a reason for you to use multiple masks. If pain is an issue, then a different mask could be used to alleviate any discomfort.
- To minimize skin breakdown by switching up masks that put pressure in different locations.
- A second mask can be used as a backup when one mask is drying or broken.
- Travel could be a factor to put multiple masks into rotation (a lighter mask may be more convenient when traveling) or for someone who lives in multiple homes (those with different homes may have multiple PAP devices, each with its own mask, at each residence).
- Mask needs may evolve over time, and significant changes in weight and skin integrity should prompt a reevaluation of mask choices.
Having a collaborative relationship with your provider is key to incorporating the best strategies as you develop the practical life-skills needed for PAP proficiency.
The following keys to successful sleep apnea self-management are important for long-term, successful treatment: (1) understanding sleep apnea; (2) understanding how CPAP manages sleep apnea on a nightly basis; (3) the importance of troubleshooting problems with CPAP therapy, such as monitoring symptoms and working collaboratively with the healthcare team; and (4) increasing the benefits while reducing the problems of using CPAP.
Where can I find a program that utilizes some of these Self-Management Educational Approaches? The best place to continue your follow up care for maximum compliance is at a comprehensive sleep center that offers one of the following services: a) a behavioral sleep therapist on staff (i.e., here and here are links to quick lookup tools for a practitioner in your area), b) a clinical sleep educator (CSE) on staff, or c) collaborates with an external A.W.A.K.E. or internal COPD sleep support group. There are over 50 active A.W.A.K.E. programs available throughout the country and many pulmonary sleep clinics hold their own COPD support groups. If you are a patient diagnosed with sleep apnea, consider getting a referral to a robust sleep disorders center and taking charge of the long-term management of your breathing disorder. Your health depends on it.
—Matthew Anastasi, BS RST RPSGT, Clinical Coordinator Consultant, Circadiance
REFERENCES
Haniffa M, Lasserson TJ, Smith I (2004). Interventions to improve compliance with continuous positive airway pressure for obstructive sleep apnoea (Review). The Cochrane Database of Systematic Reviews, Issue 4 Art No: CD003531-pub2.
Shekelle, P., Rubenstein, L., Maglione, M., Chodosh, J., Mojica, W., Morton, S., et al. (2005). Chronic disease self-management for diabetes, osteoarthritis, post-myocardial infarction care, and hypertension. Evidence report prepared for the U.S. Department of Health and Human Services. Baltimore, MD: Centers for Medicare & Medicaid Services.
Nasca TR. After the Sleep Apnea Diagnosis. Sleep Apnea. https://www.sleepapnea.org/treat/after-the-sleep-apnea-diagnosis/.
Rosenstock, I. M. (1966). Why people use health services. Milbank Memorial Fund Quarterly, 44, 94–127.





