William Golding once said, “Sleep is when all the unsorted stuff comes flying out as from a dustbin upset in a high wind.” Once thought to be a period when the brain and body shut down, we now know that sleep is very much a psychologically and physiologically active time. Sleep serves to keep the brain and body in a state of balance; and it affects everything from memory consolidation and body temperature regulation to mood and concentration, cardiac function and insulin sensitivity.
In 2017, a 15-member panel of sleep experts reviewed over 5,000 scientific findings on sleep and released the following position statement on sleep duration: Adults should sleep 7 or more hours per night on a regular basis to promote optimal health. In reality, over one-third of American adults average less than 7 hours (Centers for Disease Control, 2016), and are sleep deprived as a result.
Although there are over 100 diagnosable sleep disorders, Insomnia is the most common sleep complaint, and the second most overall in the primary care setting, behind pain (Mahowald, 1997). It has been estimated that Insomnia symptoms afflict around one-third of the US population (Bhaskar, 2016).
In an effort to manage Insomnia, there are a host of strategies for promoting Sleep Initiation (falling asleep) and Sleep Maintenance (staying asleep).
One such approach is called Stimulus Control and refers to the following three strategies:
- Sleep hygiene
- Improve daytime habits by being more active and engaged with your social networks; improve your mood; expose yourself to sunlight; limit alcohol, caffeine and nicotine.
- Encourage better sleep at night
- Naturally boost your melatonin levels; don’t read from a back-lit device at all; make sure your bedroom is quiet, dark and cool; use your bedroom only for sleep and sex; move bedroom clocks out of view.
- Keep a regular bedtime routine
- Maintain a consistent sleep schedule; block out snoring; go to bed earlier; develop bedtime rituals; limit your use of sleeping aids and sleeping pills.
Although consolidating sleep is best, there are times when napping can allow you to catch up on lost sleep which makes it our fourth strategy:
- Nap smart
- Short (15-45 minutes); early (in the afternoon); comfortable (environment).
Every cell in our bodies has its very own biological clock, ticking in unison to the 24 hour cycle of dark and light on earth. Our company, Circadiance, which comes from the Latin circa ‘about’ + dies ‘day’, is a nod to this physiological process:
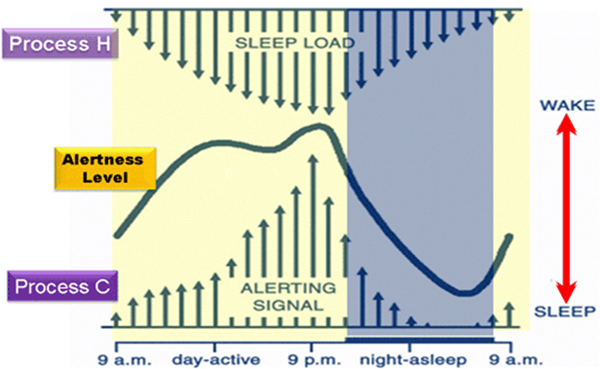
- Schedule your day around “Process C,” or the circadian rhythm times when you are most alert, and “Process H,” which refers to periods when the drive for sleep, known as the Homeostatic Drive, is weaker. The following figure indicates the Two Process Model (Borbély, 1982) showing the times when your alertness level is higher (i.e., mid-day and around 9:00pm) and when it is lower (i.e., afternoon “circadian dip”).
If you are expecting to lose sleep due to an upcoming exam, medical procedure or jet lag from a trip across time zones, this next strategy can help you mitigate the effects of sleeplessness:
- Plan for future sleep loss by “Banking Sleep”:
- For several nights before a period where you expect to lose sleep, extend the amount of time in bed to promote Sleep Saturation, which is a way of “filling up the tank” with sleep. In a 2009 study by Rupp et al., subjects with extended sleep periods under their belt performed better in alertness tasks after experiencing several nights of sleep restriction.
- The research suggests that the physiological mechanisms which contribute to sleepiness are long-term and cumulative and can be planned for by “banking sleep” in advance.
This next strategy is an example of a relaxation training approach that comes in many forms—be it mobile application, guided meditation, biofeedback or visualization:
- “The Elevator Trick”
- As you lie down to sleep, imagine you are in an elevator that goes up or down based on your level of alertness. After you feel that 20 minutes have passed, ask yourself, “Is the elevator going up or down?” If the answer is “down,” stay in bed. If not, get out of bed and do something that tires you out like reading or laundry, then go back to bed when you are sleepy and 20 minutes have passed, and try again. Repeat until you are asleep.
If the previous strategies are not enough to remedy your sleep issue, our final approaches can be performed through a consultation with a Cognitive Behavioral Therapist for Insomnia, a specialist with an entire toolbox of sleep strategies. CBT-I refers to efforts to replace thoughts about sleep and behaviors that are maladaptive. It is a validated way to promote sleep without the use of medications, relies on the previous strategies mentioned, plus the following:
- Sleep Restriction
- Use a sleep diary or sleep tracking app that establishes your typical bedtime, time to sleep, and wake up time. Change your bedtime to match your time to sleep to ensure that your homeostatic pressure to sleep (“Process H”) is at its highest, and eliminate naps. This creates one, consolidated sleep period that maximizes the percentage of time sleeping while in bed.
- Paradoxical Intention
- Involves avoiding any effort to fall asleep by remaining passively awake. The act of sleeping is the absence of effort. Counter-intuitively, worrying that you can't sleep can actually keep you awake. Letting go of this worry can help you relax and make it easier to fall asleep.
The American Academy of Sleep Medicine website allows you to search for an accredited sleep center.
The Society of Behavioral Sleep Medicine website offers a directory for finding a credentialed CBT-I provider.
We hope you have found these sleep strategies helpful so that your sleep is transformed this week! Be sure to share this blog with a friend who needs to improve on their sleep. #SleepAwarenessWeek
-Matthew Anastasi, BS RST RPSGT
References:
Watson, N. F., Badr, M. S., Belenky, G., Bliwise, D. L., Buxton, O. M., Buysse, D., Dinges, D. F., Gangwisch, J., Grandner, M. A., Kushida, C., Malhotra, R. K., Martin, J. L., Patel, S. R., Quan, S. F., & Tasali, E. (2015). Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep, 38(6), 843–844.
CDC - Data and Statistics - Sleep and Sleep Disorders. (2017, May 2). Retrieved from https://www.cdc.gov/sleep/data_statistics.html
Mahowald, M. W., Kader, G., and Schenck, C. H. (1997) Clinical categories of sleep disorders I. Continuum, 3(4), 35–65.
Bhaskar, S., Hemavathy, D., & Prasad, S. (2016). Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. Journal of family medicine and primary care, 5(4), 780–784.
Watson, N.F. (2016). Health care savings: the economic value of diagnostic and therapeutic care for obstructive sleep apnea. J Clin Sleep Med, 12(8), 1075-1077.
Borbély, A. A. (1982). A two process model of sleep regulation. Human Neurobiology, 1(3), 195–204.
Rupp, T. L., Wesensten, N. J., Bliese, P. D., & Balkin, T. J. (2009). Banking sleep: realization of benefits during subsequent sleep restriction and recovery. Sleep, 32(3), 311–321.





