Using CPAP during a public health emergency like the COVID-19 pandemic means navigating potential infection risks posed through a process called AGP or aerosol generating procedure, of which CPAP is an example. To this end, we have compiled the most effective approaches that address the three scenarios of concern that are most often voiced by patients during the pandemic.
- Does CPAP increase my chance of getting infected?
If a bedpartner were to be positive for Covid, there is no evidence CPAP potentiates infection in the user. However, it is undeniable that the virus does not change a sleep apnea diagnosis – or the need to continue using CPAP therapy. In fact, quite the opposite: sound sleep improves immune function, and patients with OSA are at up to 2.8x higher risk of death when contracting the virus according to a recent systematic review of 18 studies by Michelle Miller.¹¹ Although the benefits of CPAP outweigh the risks there is still a cost/benefit decision to be made between patient and provider. And, if a pause in CPAP is determined, there are temporary alternative OSA treatments available other than the gold standard, including oral appliance therapy (OAT) and positional therapy (PT). - Can I be re-infected from my CPAP?
Covid + PAP users should follow manufacturer cleaning recommendations for the mask diligently to prevent re-infection, but there is also the CPAP machine itself, and tubing to address. Disposable tubing should be used and replaced as often as possible (tubing is notoriously difficult to clean and dry completely, and disposable tubing is cheap), and the CPAP machine air intake filter should be replaced frequently as well. There is also the humification chamber to address. Sleep labs running titrations are either not using them altogether or throwing them out after each use during the pandemic, due to difficulty disinfecting them. Single use patients at home should thoroughly clean according to the manufacturer and use sterile or distilled water instead of tap water. Additional recommendations include reminder to wash your hands before handling your mask. - Does my CPAP use increase the chance that a family member will acquire the virus?
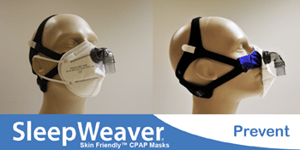
A Covid+ person should isolate whether or not (s)he is using CPAP, to prevent the spread of infection, especially in multi-generational homes where at-risk family members may be present. Theoretically, the risk from CPAP is from the aerosol spread of virus particles from the lungs that leak around the mask seal, anti-asphyxiation valve, and through the exhalation port of the mask. The Circadiance SleepWeaver Prevent has received FDA emergency use authorization during the pandemic to address these risks. It uses a combination approach to reduce virus particles: the CPAP mask is covered by a KN95 mask that is integrated around the swivel elbow, essentially filtering any exhaled air before it reaches the atmosphere. You can learn more about this new approach to reducing the risk by watching this brief instructional and fit video.
The A.W.A.K.E. network is a patient education and support group hosted by the American Sleep Apnea Association (ASAA) and with over 50 meeting locations throughout the country. There are also a variety of online support groups called forums where patients can interact virtually by asking other CPAP users and sleep professionals questions about therapy and diagnosis. The forums are set up like message boards for different categories and you can post your question and receive answers. These forums are usually very supportive and moderated (for good behavior and to make sure users follow the forum rules). Even if you don’t set-up your own account (which is usually free) you can view the message boards as a guest and search for questions that other users have asked that may help you.¹² These include Apnea Board, CPAP Talk, MyApnea, Free CPAP Advice Forum, and the ASAA Sleep Health Forum.¹³
All things considered, life does change with CPAP. For the better. The old saying goes that the hardest thing to do in life is change. But consider the alternative.
—Matthew Anastasi, BS RST RPSGT, Clinical Coordinator Consultant, Circadiance
REFERENCES
¹ Watson NF. Health Care Savings: The Economic Value of Diagnostic and Therapeutic Care for Obstructive Sleep Apnea. J Clin Sleep Med. 2016;12(8):1075-1077. Published 2016 Aug 15
² ‘CPAP Machine Changed My Life'. MedicineNet. https://www.medicinenet.com/script/main/art.asp?articlekey=158679. Published May 29, 2012.
³ Epstein LJ; Kristo D; Strollo PJ; Friedman N; Malhotra A; Patil SP; Ramar K; Rogers R; Schwab RJ; Weaver EM; Weinstein MD. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 2009;5(3):263–276
⁴ Anastasi MW. Chapter 46: Positive Airway Pressure Therapy: Basic Principles. In Lee-Chiong TD, Mattice C, Brooks R, eds., Fundamentals of Sleep Technology. 3rd ed. Wolters Kluwer Health, Inc., 2019:580-587.
⁵ Brandon Peters MD. What Side Effects to Expect From CPAP Therapy. Verywell Health. https://www.verywellhealth.com/cpap-therapy-what-are-the-side-effects-3015024.
⁶ Lewis KE et al. (2004). Early predictors of CPAP use for the treatment of sleep apnea. Sleep, 27, 134-138.
⁷ Krakow, B, et al. (2008). A daytime, abbreviated cardio-respiratory sleep study to acclimate insomnia patients with sleep disordered breathing to positive airway pressure (PAP-NAP). J Clin Sleep Med, 4,212-22.
⁸ Anastasi M, Pasquale M, Tubbs A. Comparison of PAP Interface Pressure on the Nasal Bridge: Soft Cloth vs. Traditional Masks. Abstract submitted for publication. 2020.
⁹ Perez C. Managing Multiple Masks. Sleep Review. https://www.sleepreviewmag.com/uncategorized/managing-multiple-masks/. Published August 19, 2015.
¹⁰ Young, T., Finn, L., Peppard, P. E., Szklo-Coxe, M., Austin, D., Nieto, F. J., et al. (2008). Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin sleep cohort. Sleep, 31(8), 1071-1078.
¹¹ Miller MA, Cappuccio FP. A systematic review of COVID-19 and obstructive sleep apnoea. Sleep Medicine Reviews. https://www.sciencedirect.com/science/article/pii/S1087079220301258?via=ihub. Published September 8, 2020.
¹² Michaud L. 4 realities of life with sleep apnea and living with your CPAP Machine. https://www.alaskasleep.com/blog/4-realities-of-life-with-sleep-apnea-living-with-your-cpap-machine.
¹³ Rodriguez J. Best Online CPAP Support Groups and Resources. Advanced Sleep Medicine Services, Inc. https://www.sleepdr.com/the-sleep-blog/best-online-cpap-support-groups-and-resources/. Published December 7, 2016.





