The three pillars of optimal health are nutrition, physical fitness, and sleep. Think of your health as stabilized on a chair. Taking any one of the legs away would topple the seat, so tending to each section is essential to living well.
The reality of our collective sleep debt, and the health implicationsIn 2015 (1), a panel of sleep experts convened a position statement on how much sleep is needed. They pored through thousands of scientific articles and came up with a recommendation of 7 or more hours.
The conclusion is significant because in the 50 year history of sleep science, no one had undertaken a project to answer this question.
Despite this consensus statement, Americans are not getting enough sleep, and it shows. According to the CDC (2), more than a third of adults do not get the recommended 7 hours.
The prevalence of “short sleepers” can be higher or lower based on your location, shown in the following figure showing incidence by county, from the CDC (3):
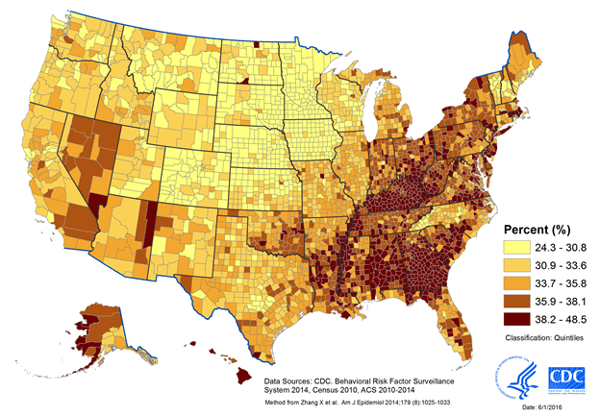
Sleeping <7 hours per night is associated with a host of increased health risks including obesity, diabetes, high blood pressure, heart disease, stroke and more (4–6).
Moreover, the quantity of sleep is not the only factor, it turns out the quality of sleep matters even more. In addition to the health risks of insufficient sleep, poor quality sleep also impairs cognitive performance, leading to an increase in the likelihood of accidents and loss of productivity, which can have widespread indirect effects on the community at large (7).
Insomnia
Insomnia is the second most common complaint, after pain, in the primary care setting (8).
It is the most prevalent sleep disorder. 70 million people have symptoms of Insomnia in the U.S., and 30% to 50% of Americans report the sleep difficulty in a given year.
There is a quick way to screen yourself for Insomnia. Do you have trouble falling asleep, staying asleep, or get up too early? A disturbance of more than 30 minutes at either of these three times along with daytime sleepiness puts you at risk for Insomnia. If you need alcohol or medication to get to sleep, you are also at risk for Insomnia.
The recommended first-line treatment is Cognitive Behavioral Therapy for Insomnia or CBT-I. This approach involves use of three techniques in a brief, 4-6 session (once/week) intervention:
- Stimulus Control
- The bedroom should be a place for relaxation. This is a strategy to pair one’s awareness as the bedroom as a cue for sleep and disconnect associations that promote wakefulness. For example, stimuli such as television and other screens are removed to allow a patient to be conditioned to the bedroom in way that reduces anxiety.
- Sleep Restriction
- Quality is more vital than quantity in this approach. This step-wise procedure aims to consolidate a sleep period by initially restricting the amount of sleep that is currently feasible. In subsequent weeks the time spent in bed is gradually increased.
- Sleep Hygiene
- Patients with Insomnia typically have maladaptive behaviors toward good sleep. Sleep Hygiene includes all daytime activities that set you up for a successful night like avoiding naps > 30 minutes, skipping afternoon stimulants, and being exposed to natural light. In the evening, the goal is to shift from “trying to sleep” to “allowing sleep to happen” by making sure your sleep environment is pleasant and establishing a bedtime routine.
Obstructive Sleep Apnea
Most people with Obstructive Sleep Apnea (OSA) don’t know it. There is a saying that those who snore always fall asleep first!
The American Academy of Sleep Medicine (AASM) recently contracted a global research and consulting firm to uncover the economic costs of untreated sleep apnea for payers, employers and patients. They found that only 20% of Americans with OSA have been diagnosed. Out of the diagnosed, only 50% are compliant with treatment. By these figures < 10% of those suffering from sleep apnea are effectively treated! The economic impact of this was found to be $149.6 billion (9).
54 million Americans are estimated to suffer from OSA (10), the second highest number in the world (after China, estimated to have 176 million cases).
With the population aging and becoming more obese, OSA will continue to see an increase in cases. According to the CDC, nearly 80 percent of adults and about one-third of children now meet the clinical definition of overweight or obese. More Americans live with “extreme obesity“ than with breast cancer, Parkinson’s, Alzheimer’s and HIV put together.
For a quick screening to determine OSA risk, ask yourself:
- Have I been told I snore loudly (louder than talking or loud enough to be heard
through closed doors)? - Do I often feel tired, fatigued, or sleepy during daytime?
- Has anyone observed me stop breathing during sleep?
- Do I have or am I being treated for high blood pressure?
YES TO TWO OR MORE = YOU ARE AT HIGH RISK FOR SLEEP APNEA
Positive Airway Pressure (PAP) therapy is the gold standard and most widely used treatment for OSA. PAP is recommended by the AASM in the treatment of moderate (defined as ≥ 15, but < 30 breathing pauses lasting 10 seconds or more, per hour sleep) to severe (≥ 30 events per hour) obstructive sleep apnea in adults, and an option for the treatment of mild (≥ 5, but < 15 per hour) sleep obstructive sleep apnea.
PAP therapy introduces positive pressure to the airway by first delivering pressurized air to the nose and/or mouth through an “interface” or mask is held in place by straps that form the “headgear.”
PAP therapy has been associated with significant improvements in health measures. A meta-analysis (12) of 336 studies concluded that “The data demonstrated that PAP compared to no treatment results in a clinically significant reduction in disease severity, sleepiness, blood pressure, and motor vehicle accidents, and improvement in sleep-related quality of life in adults with OSA.”
Sleep disorder treatments increasingly turn to “Precision Medicine”
Sometimes called “Personalized” Medicine, Precision Medicine is an approach which takes into account individual differences to allow for tailored treatments that target the unique needs of each patient. It does this by taking into account a patient’s set of challenges to anticipate their needs. This has the two-fold benefit of preventing waste and improving patient outcomes.
The goals of clinical Precision Medicine are to improve the quality of patient care, enable cost-effectiveness, and reduce readmission and mortality rates. This improves our ability to predict which treatments will work best for specific patients. Some recent examples of using tools from Precision Medicine in Sleep Medicine include:
- Mask selection algorithms to increase the success of first choice interfaces and for remote fitting
- CBT-I for Insomnia
- Oral Appliance Therapy for mild to moderate levels of OSA
- Weight loss for OSA patients with severe obesity
- Implantable hypoglossal neurostimulation (HGNS) for patients who are non-compliant with CPAP
- Medications for narcolepsy patients
- Positional Therapy for POSA (Positional Obstructive Sleep Apnea, which is Sleep Apnea that primary occurs when laying on the back)
- Combination therapy to compound the effectiveness of multiple approaches
Where do I find help?
The American Academy of Sleep Medicine allows you to search for a certified sleep center here: http://sleepeducation.org/find-a-facility
The Society of Behavioral Sleep Medicine website offers a directory for finding a CBT-I behavioral sleep medicine provider here: https://www.behavioralsleep.org/index.php/united-states-sbsm-members
REFERENCES
1. Watson NF, Badr MS, Belenky G, et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843-844.
2. Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of Healthy Sleep Duration among Adults — United States, 2014. MMWR Morb Mortal Wkly Rep 2016;65:137–141.
3. CDC - Data and Statistics - Sleep and Sleep Disorders. Centers for Disease Control and Prevention. https://www.cdc.gov/sleep/data_statistics.html. Published May 2, 2017.
4. Grandner MA, Chakravorty S, Perlis ML, Oliver L, Gurubhagavatula I. Habitual sleep duration associated with self-reported and objectively determined cardiometabolic risk factors. Sleep Med 2014;15:42–50.
5. Liu Y, Wheaton AG, Chapman DP, Croft JB. Sleep duration and chronic diseases among US adults age 45 years and older: evidence from the 2010 Behavioral Risk Factor Surveillance System. Sleep 2013;36:1421–7.
6. Gallicchio L, Kalesan B. Sleep duration and mortality: a systematic review and meta-analysis. J Sleep Res 2009;18:148–58.
7. CDC. Perceived insufficient rest or sleep among adults—United States, 2008. MMWR Morb Mortal Wkly Rep 2009;58:1175–9
8. Sateia, M.J., et al., Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med, 2017. 13(2): p. 307-349
9. Watson NF. Health Care Savings: The Economic Value of Diagnostic and Therapeutic Care for Obstructive Sleep Apnea. J Clin Sleep Med. 2016;12(8):1075-1077. Published 2016 Aug 15.
10. Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7(8):687-698.
11. Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of Adult Obstructive Sleep Apnea with Positive Airway Pressure: An American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med. 2019;15(2):335-343.
12. Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of Adult Obstructive Sleep Apnea With Positive Airway Pressure: An American Academy of Sleep Medicine Systematic Review, Meta-Analysis, and GRADE Assessment. J Clin Sleep Med. 2019;15(2):301-334.





